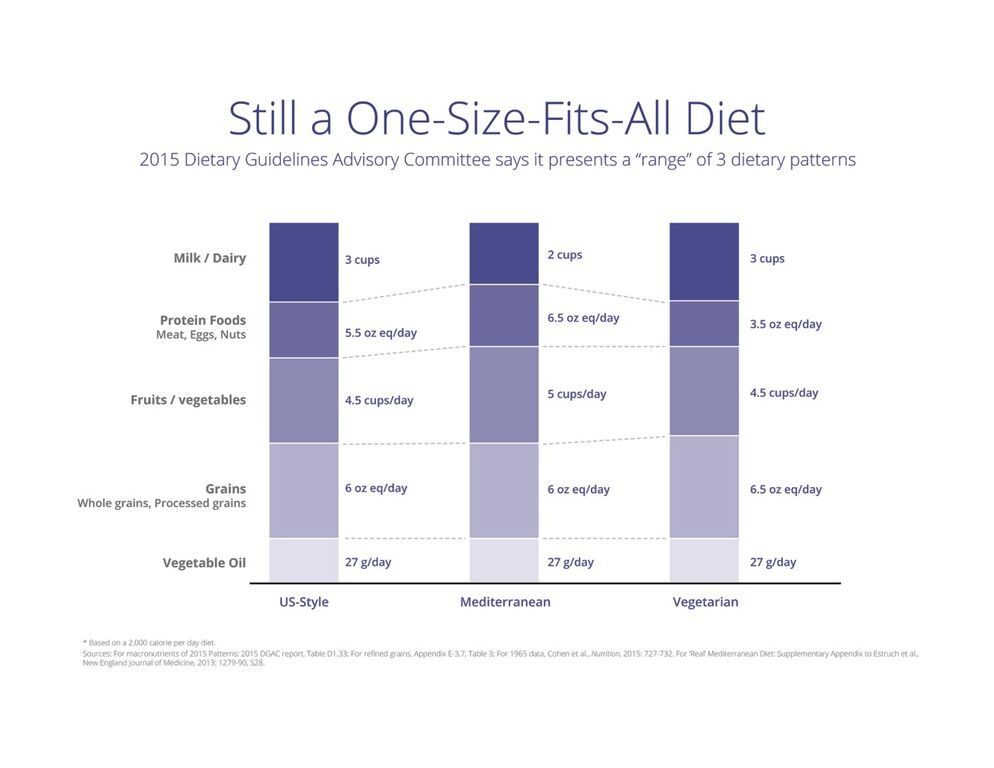
For much of modern nutrition history, a rather large assumption/concept has dominated thinking by experts in nutrition as well as in the general population: the “one-size-fits-all diet“. An example is the U.S. government food pyramid, or the current iteration “MyPlate”. Almost every government peddles some version of this – and sadly most are wrong… just look at the pandemic of metabolic diseases plaguing our planet.
In reality, current science supports the idea that nutrition plans and diets should be tailored for individuals, their culture, genetics, microbiome, environmental exposures, metabolic health, etc. Science supports using data to make decisions about what you eat, not fads, macronutrient ratios, etc. Modern nutrition science requires us to learn some actual science, use validated information to support decisions about what we eat, and last but not least, to cook and eat whole, real food (not food-like products and additives).
This means, when you hear someone tell you how to manage your blood sugar by giving you rote directions from a standardized diet plan, or worse yet, proffers some half-baked diet philosophy, commercialized proprietary food product regimen, or snake oils in form of expensive supplements, health-shakes, etc., then walk away. Some may do better on a low-fat diet, some on a low-carb diet, some on plant-based foods, and others on an animal-based foods – or all of the above. Don’t let food fanatics and philosophers, and with all due respect, kettlebell instructors, mislead you about what is good for you.
Added sugar? Processed carbohydrates? That isn’t food or nutrition, so it is a “no-brainer” to cut these out.
Regrettably, some (many) healthcare institutions and providers don’t have a clue about nutrition – just look at the last meal you had in a hospital – either as a patient or as a visitor. Less than 30% of doctors are required to take a nutrition course during medical school. This means you have to shop around, find the right expert to guide you: someone who uses actual data, and then tailors a plan for you based on what the data and the science say, not their opinion or belief system. It is relatively easy to sort out the charlatans from the professionals – the professionals gather information, ask questions, and then formulate a plan… the charlatans just prescribe the same thing to all their patients, like you are a member of a herd. Don’t be part of the herd – be heard!
Below, we share a few articles and resources for you to get acquainted with this issue.





Recent Comments