Another Tragic and Unrecognized Aspect of Hypoglycemia – Its Connection to Alcoholism
An often overlooked aspect of alcoholism: its relationship to your blood sugar and diet
“I have never, ever seen an alcoholic who was not hypoglycemic.
It just doesn’t occur; it’s the same problem.”
-Dr. Douglas M. Baird
Dr. Douglas M. Baird, a physician in South Florida, brought the hypoglycemia-alcoholism connection to light in his first presentation for the Hypoglycemia Support Foundation (HSF) in 1982, where this one pronouncement, to a spellbound audience, made a powerful and lasting impression.
Dr. Joan Mathews-Larson, author of 7 Weeks to Sobriety, which has a highly informative section on hypoglycemia detailing the results of thousand Glucose Tolerance Tests (GTTs), agrees wholeheartedly with Dr. Baird’s assertion. In an illuminating interview she had with Dr. Julian Whitaker, she stated: “It is an absolute must that alcoholics change their diet to control their hypoglycemia or they will never get their alcoholism under control…It is very clear that the success rate in stabilizing alcoholism is shamelessly low because one of the main contributing factors, hypoglycemia, is not being addressed.”
Dr. Larson’s paper on Alcoholism Treatment with Biochemical Restoration as a Major Component is considered to be a classic among those who believe addressing nutrient deficits are just as important, if not more so, than “talk therapy” in addressing addiction. Dr. Larson is to be lauded for being among the first to examine the connection between hypoglycemia and alcoholism and to see hypoglycemia as an indicator of nutrient deficiencies that underlie the urge to drink alcohol, not merely as a symptomatic condition of alcoholism.
Mark Mathews shares this in “The Centerpiece of Alcoholism: “Dr. John Tintera, Charter Member of the New York Commission on Alcoholism and endocrinologist stated, “the treatment of alcoholism centers on the control of hypoglycemia. By far the most important part of physiologic treatment is the complete restriction of easily absorbed carbohydrates.” He went on to warn, until severe blood sugar fluctuations are stabilized, “alcoholic’s will be predisposed to depression and what only appears to be deep rooted emotional and psychiatric disorders.” That was over 40 years ago, but it’s still not taught in schools that train licensed Alcohol/Chemical Dependency Counselors.”
Dr. Baird states that “Alcoholism, like hypoglycemia, can be related to a faulty metabolism. Preliminary physical and dietary evaluations should be completed as well as blood glucose testing. The chemical imbalance created by years of poor dietary habits can be brought back into alignment with implementation of proper diet, vitamin therapy and lifestyle changes. Such a program can stabilize the alcoholic’s blood sugar and thus make it easier for the alcoholic to maintain abstinence.”
Dr. Baird and Dr. Larson aren’t alone; there are many others who also make the connection between alcoholism and hypoglycemia clear:
According to James R. Milam, Ph.D. and Katherine Ketcham in their book Under The Influence, “While the diagnosis of hypoglycemia may be mistakenly used by people to explain unrelated psychological and emotional problems, there is no question that the great majority of alcoholics suffer from chronic low blood sugar. When given the 5-hour glucose tolerance test, over 95 percent of both early- and late-state alcoholics experience a spike in blood sugar after intake of sugar and then a rapid plunge.”
In the New Diet Revolution, Dr. Robert C. Atkins states, “Experience shows that when an alcoholic succeeds in getting off alcohol, he usually substitutes sweets. This is because almost all alcoholics are hypoglycemic, and sugar provides the same temporary lift that alcohol once did.”
In Hypoglycemia: The Classic Healthcare Handbook, Dr. Harvey M. Ross laments the “plethora of doctors and counselors who ignore the results of the research that proves that the alcoholic has a blood sugar problem.”
Dr. David G. Williams states in Hypoglycemia: The Deadly Roller Coaster: “To combat alcohol and other drug abuse, abstinence, proper diet, nutritional supplementation and education about abuse and hypoglycemia must be part of the program.”
Dr. Alexander Schauss in Diet, Crime and Delinquency suggests that if you treat the alcoholics for hypoglycemia there can be a success rate as high as 71% compared to 25% for approaches like AA.
Dr. Thomas Mackenzie states in his 1979 paper, Hypoglycemia and Alcoholism, “The effect of alcohol on blood sugar must be distinguished from the effect of blood sugar fluctuations on the urge to imbibe. The first instance deals with the question of whether alcohol can precipitate hypoglycemia. The second relates to whether preexisting hypoglycemia can cause alcohol use. Apparently independent of its properties as an hepatotoxin, alcohol can cause fasting hypoglycemia by selectively inhibiting gluconeogenesis. There are two hypothetical mechanisms by which ingestion of alcohol might relieve the symptoms of hypoglycemia and thus be operantly reinforced. First, alcohol might result in the additional availability of glucose; and second, alcohol might mitigate the physiologic symptoms of hypoglycemia (for example, tremor, diaphoresis, tachycardia, nervousness) via its centrally acting anxiolytic properties. If reactive hypoglycemia is suspected in an alcoholic patient, evaluation cannot be undertaken until alcohol intake has been discontinued and a normal diet begun. If a careful medical history and thorough physical exam do not clarify the situation, a five-hour glucose tolerance test should be ordered.”
Dr. John D. Tintera, M.D concluded after years of research that even recovered alcoholics who have been sober for many years continue to suffer the effects of hypoglycemia and states that “…by far the most important part of the physiological treatment of alcoholics is the complete restriction of easily absorbed carbohydrates.”
Dr. Elsa Colby-Morley, in the paper “The Reflection of Hypoglycemia and Alcoholism on Personality: Nutrition as a Mode of Treatment” shares Dr. Roger Williams perspective that “It is quite possible that malnutrition develops as a forerunner of alcoholism, and that it is only when malnutrition of the brain cells becomes severe that true alcoholism appears.” Dr. Williams asserts that “no one who follows good nutrition practices will ever become an alcoholic.” Dr. Colby-Morley states: “Alcohol may, if taken in large enough quantities, actively damage the brain cells as well as deprive the brain cells of the necessary items in the nutritional chain of life.” Dr. Colby-Morley notes that “Most hypoglycemics have a ravenous appetite for sweets. Since the overactive pancreas— which spurs the desire for sweets— will be restimulated when sugar is eaten, this illustrates an aberration of the ‘wisdom of the body.’ Characteristic of a group of alcoholics is this same desire for sweets; while sober they consume unbelievable quantities of candy, cookies and sugar in their coffee. The craving for sweets is a clue to low blood sugar. Meals are often made up of “junk” foods that are high in refined carbohydrates, fats, and salt: low in high quality protein, and devoid of fresh fruits and vegetables and whole grains. This type of diet can lead to blood sugar instability in susceptible individuals and, indeed, it is claimed upwards of 95 percent of alcoholics suffer from low blood sugar (Meiers. 1973). From all the facts relating alcoholism to biological factors and nutritional deficiencies, it becomes clear that whatever measures may be taken to prevent alcoholism, the neglect of the nutritional approach cannot be justified. (Roger J. Williams. 1971).
What’s on Your Plate? The Power of Nutrition for those in Recovery
“The prevalence of hypoglycemia in alcoholics has been well established. One condition reported among alcoholics is hypoglycemia. The symptoms of hypoglycemia reported resemble those referred to as the “dry drunk,” including: grogginess, sleepiness, depression, extreme fatigue, food cravings (e.g. alcohol, sugar, etc.), mental confusion, etc.” – Joan Mathews-Larson, Ph.D. and Robert A. Parker, M.Sc., Alcoholism Treatment with Biochemical Restoration as a Major Component
“At least 80% (if not more) of all alcoholics, (Milam) premenstrual women, those who habitually eat large amounts of sugar/refined carbohydrates, and patients from alcoholic families, have dysregulated blood sugar metabolism, termed reactive hypoglycemia by many in the health professions. In these cases, the pancreas appears to release excessive amounts of insulin, lead.ing to a precipitous drop in blood sugar, which then may even fall below the normal baseline. Two very significant metabolic changes happen at this point. First, the adrenal gland releases adrenaline in an attempt slow down this precipitous drop, by stimulating the release of some stored sugar back into the bloodstream. Second, as the drop in blood sugar continues, the now starving and unbalanced brain sends out urgent signals for the body to do whatever it takes, to bring blood sugar levels back into balance. This message can easily translate into a powerful craving for quick energy sources such as alcohol or sugar, but this signal just as easily could lead to a craving for the drug or addictive behavior of choice, since an addict’s brain has previously been conditioned to look to its drug of choice to restore equilibrium. Thus, the alcoholic craves alcohol, the sugar addict craves sugar, the smoker craves a cigarette, and the sex addict craves sex! This relapse-inducing craving especially occurs if a meal is missed, and simply too much time has passed since the brain has last been fed.” – Christina Veselak, LMFT, Relapse and Blood Sugar Dysregulation
Julia Ross, Advisor to the HSF, author of The Craving Cure and The Mood Cure, and a recovery expert with decades of experience working with alcoholics, explains the issues so well: “Another of the primary reasons people get addicted to alcohol is that their blood sugar levels tend to drop too low, too often. Over 95% of alcoholics are hypoglycemic. When they experience a drop in blood sugar, the code red “get a drink” signal turns as the brain begins to fail from a lack of fuel. No amount of willpower alone can turn it off. Reversing hypoglycemia is a vital job if you’re going to successfully escape alcoholism. The anti-alcohol diet emphasizes high-protein foods rich in amino acids. Substituting protein for simple carbohydrates helps break the vicious cycle of blood sugar cravings, and the amino acids are key to brain function. We’re giving the brain certain foods so it can make the natural chemicals we need to feel happy.”
It is important to note that sugar and alcohol have similar effects in terms of how they are metabolized. Sugar is now in 75% of our food supply; how might this reality be affecting us? Dr. Robert Lustig, Medical Advisor to the HSF, is keen to educate the general public that one of the most common forms of sugar added to processed food and beverages is fructose. Unlike glucose, which can be used by virtually every cell in your body, fructose can only be metabolized by your liver, because your liver is the only organ that has the transporter for it. Since all fructose gets shuttled to your liver, and, if you eat a typical Western-style diet, you consume high amounts of it, fructose ends up taxing and damaging your liver in the same way alcohol and other toxins do.
In fact, Dr. Lustig points out that fructose is virtually identical to alcohol with regard to the metabolic havoc it wreaks. According to Dr. Lustig, fructose is a “chronic, dose-dependent liver toxin.” And just like alcohol, fructose is metabolized directly into fat – not cellular energy, like glucose. Dr. Lustig explains the three similarities between fructose and its fermentation byproduct, ethanol (alcohol):
- Your liver’s metabolism of fructose is similar to alcohol, as they both serve as substrates for converting dietary carbohydrate into fat, which promotes insulin resistance, dyslipidemia (abnormal fat levels in the bloodstream), and fatty liver
- Fructose undergoes the Maillard reaction with proteins, leading to the formation of superoxide free radicals that can result in liver inflammation similar to acetaldehyde, an intermediary metabolite of ethanol
- By “stimulating the ‘hedonic pathway’ of the brain both directly and indirectly,” Dr. Lustig noted, “fructose creates habituation, and possibly dependence; also paralleling ethanol.”
Dr. Lustig concludes: “Thus, fructose induces alterations in both hepatic [liver] metabolism and central nervous system energy signaling, leading to a ‘vicious cycle’ of excessive consumption and disease consistent with metabolic syndrome. On a societal level, the treatment of fructose as a commodity exhibits market similarities to ethanol. Analogous to ethanol, societal efforts to reduce fructose consumption will likely be necessary to combat the obesity epidemic.”
“ I don’t hide it, I am an alcoholic! I’ve tried everything I could for the past 20 plus years to kill this “devil” in me! I actually gave up hope that I would find an answer or a cure. Then I accidentally came across your book (Do’s and Don’ts of Hypoglycemia). It was on the table in a friend’s house that I was visiting. While he was in the kitchen, I picked it up and browsed through the pages, came across the chapter on the correlation between Hypoglycemia & Alcoholism and it stopped in my tracks. I asked to borrow the book, came home and read it. It transformed my life! I still have a long way to go but realize now that unless I change my eating habits, there’s little chance of recovery. The sugar and caffeine have to go! I’ve been encouraged to reach out for help. Without your book and my new direction, I have no idea where I would be today!” -Letter received by the Hypoglycemia Support Foundation
An addiction medicine review article titled “Are sweetened drinks a gateway to alcohol addiction?” reports that “Increased use of sugar and its alternatives (like High Fructose Corn Syrup or HFCS) is the largest contributor to the so called silent killer Nonalcoholic Steatohepatitis (NASH) via unexpected cardiovascular thrombotic events, diabetes, hypertension, dyslipidemia, and possibly, colon and breast cancers. Alcohol also produces Fatty Liver, with similar consequences. Therefore combining sugar in alcoholic drinks provides a ‘double whammy’ in terms of morbidity and premature sudden death.”
How far have we come in the past four decades that this information has been circulating? Roberta Ruggiero addresses this issue in the 5th edition of The Do’s and Don’ts of Hypoglycemia: An Everyday Guide to Low Blood Sugar (2017):
“Alcoholism. No one is immune to it. It doesn’t discriminate on the basis of race, religion, gender, or socioeconomic status. Sadly enough, there are also no age barriers. Whether it is used as a chemical, drug or food, 14 million Americans are under its influence. From the womb to the grave, alcohol’s effects on the body can be devastating. Its physical and emotional effects can range from upsetting the metabolism and nutritional state of the body to increasing the risk of cancer, liver and heart disease, high blood pressure, and diabetes. Erection problems may arise and, as a consequence, the need for . It can cripple the emotions with low self-esteem and promote feelings of isolation, rejection, loneliness, hopelessness, and fear. There is an abundance of literature that indicates that alcohol consumption during pregnancy can put the unborn child at risk for numerous health problems. Even if the child appears unscathed by a pregnancy where alcohol was used, this “healthy” child still has a 30 percent chance of trying alcohol by the time they are nine years old.”
Children who make it through high school without experimenting with alcohol, may not resist the temptation through college. Consider alarming statistics from the College Drinking website, where researchers estimate that each year:
- 1,825 college students between the ages of 18 and 24 die from alcohol-related unintentional injuries, including motor-vehicle crashes.
- 696,000 students between the ages of 18 and 24 are assaulted by another student who has been drinking.
- 97,000 students between the ages of 18 and 24 report experiencing alcohol-related sexual assault or date rape.
- Roughly 20 percent of college students meet the criteria for an AUD.
- About 1 in 4 college students report academic consequences from drinking, including missing class, falling behind in class, doing poorly on exams or papers, and receiving lower grades overall.
Information on alcoholism and treatment options is available just about everywhere—in newspapers, magazines, on the internet. The problem is so pervasive and devastating that individuals, communities, and businesses have come together to try to combat and educate people about the disease. Organizations such as Mothers Against Drunk Driving (MADD), and Students Against Destructive Decisions (SADD)—are involved with educating the public about the deadly combination of drinking and driving and advocating for harsher laws for offenders.
And of course, the most well-known organization helping people cope with alcoholism is Alcoholics Anonymous, which has been providing education and assistance for years. Bill Wilson, co-founder of Alcoholics Anonymous, was interested in the biochemical basis of alcoholism and addiction. It is reported that he personally suffered from hypoglycemia and depression and was known to consume a lot of caffeine and sugar. Bill W. collected research papers showing the extent of abnormal blood sugar levels among alcoholics and sent three different reports on the subject to Alcoholics Anonymous physicians. In 1968, Bill W. wrote a 48-page booklet for physicians encouraging the adoption of the hypoglycemia diet and vitamins, especially B-3, in the treatment of alcoholism. Abram Hoffer, M.D., Ph.D., writes, “Bill Wilson (co-founder of AA) began to take niacin (B-3) in a dose of 3,000 mg daily. Within a few weeks, fatigue and depression, which had plagued him for years, were gone.”
It would seem that all the information we want about alcohol use/abuse is right at our fingertips. Unfortunately, most of this information fails to acknowledge the connection between hypoglycemia (low blood sugar) and alcoholism.
Current statistics regarding the rise of alcoholism indicate that we have not come very far. Where do we go from here? The HSF believes if you want to dramatically increase your chances of controlling addiction to alcohol, it is vital to address dietary habits and to look at what is going on with your blood glucose.
It is well-established that alcohol causes hypoglycemia. Have you tried to stop drinking but experienced the following sensations: tremors, weakness, sweating, increased reflexes, gastric symptoms and seizures – even visual or auditory hallucinations? These symptoms often prevent alcoholics from quitting or cause them to replace alcohol with sugar, high carbohydrates, caffeine and/or tobacco.
But what if poor diet and blood sugar issues cause alcoholism, or at the very least, the ideal conditions for it?
Dorothy Mullen, who holds a Masters Degree in Addiction Recovery, started the acclaimed Suppers Programs to help people to achieve long term sobriety. In an illuminating video interview focused on recovery from alcoholism, Dorothy shares:
“All the work I do relates to blood sugar, the effects of blood sugar.”
“In the early days/weeks/months of sobriety, there’s a lot of band-aid eating and drinking…coffee, cookies, baked goods, donuts…they work in the short run and are what I call nutritional “harm reduction” – it’s better to eat a lot of coffee, cake and cookies than to be an active alcoholic, nevertheless it creates problems for people because they’re not going to be able to repair all the damage to digestion and all the damage to their brains if they don’t start absorbing nutrients from their food and eating in a way that gives them the building blocks for good brain function, instead of just fuel, fuel, fuel, fuel…because the newly recovered alcoholic just wants fuel and stimulants.”
How does eating well help make sobriety more comfortable?
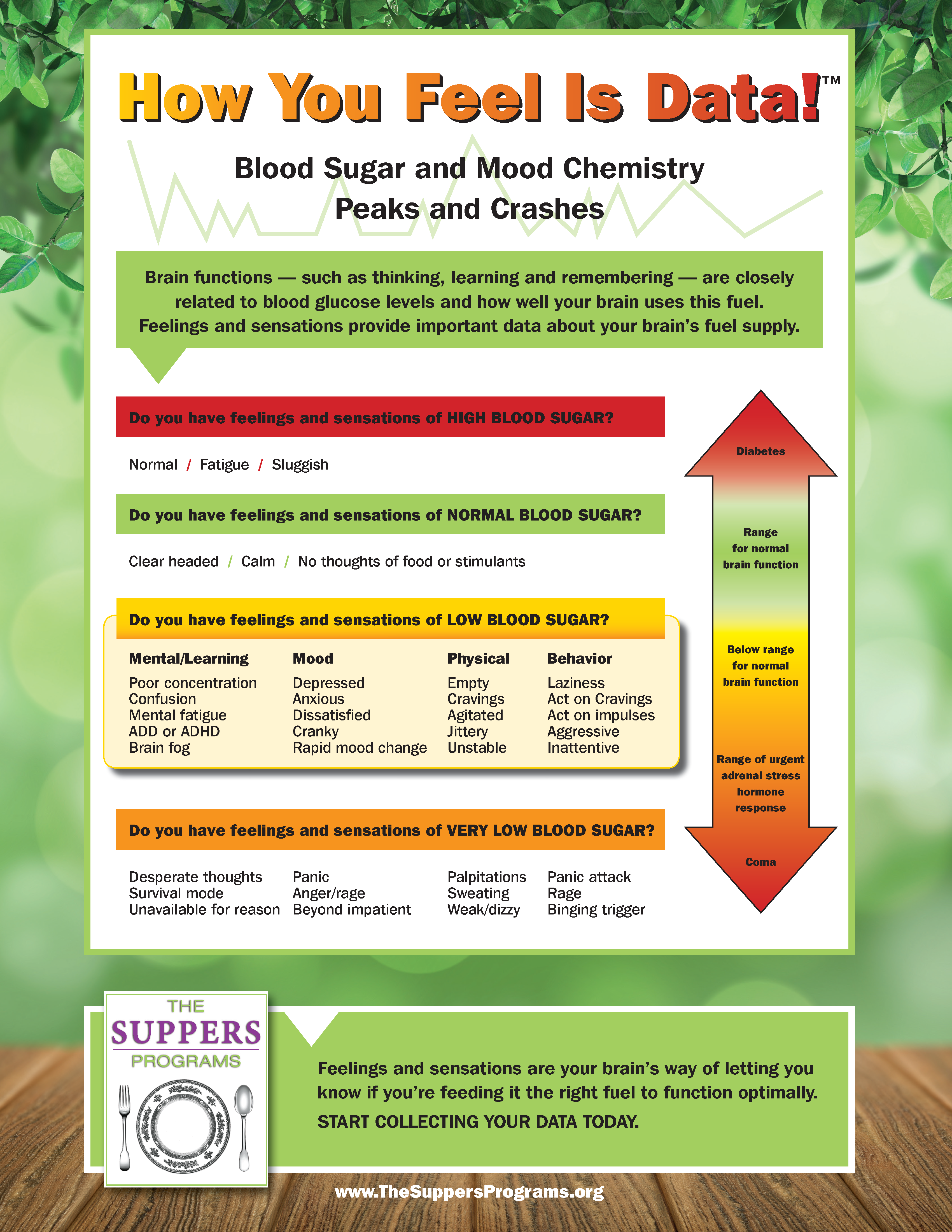
Mullen says: “I think it has to do with the “building blocks” vs. the “fuel” problem. In our diet there are certain fats and proteins that provide building blocks, and fiber is good for the digestion, and carbohydrates are all the fuel. There is a certain flaw, probably owing to food processing – we don’t have normal reactions to natural foods anymore. This flaw that occurs makes it so that no matter what we need, we go into an emergency mode…and emergency mode is always associated with “I’ve gotta get glucose,” “I’ve gotta get sugar into my bloodstream.” It’s the fight or flight mechanisms are all about having that ready energy. So, a recovering alcoholic might really need the proteins for the amino acids for good neurons-transmitters. An alcoholic will definitely need the essential fatty acids because over 60% of the dry weight of your brain is fat and we want the brain to be made out of these beautiful natural fats – and if they don’t get it, they are just going to get signals over and over and over again to put in the carbohydrates that bring them comfort and if you look at the “How you feel is data chart” (see image below) you’re going to see the same spectrum you would see for an ADD child or a person who’s becoming diabetic, starting with mental symptoms, confusion, mental fatigue, sometimes crankiness and irritability that comes because the brain is out of fuel. So we want to get these beautiful fats and proteins into these folks rather than all the fuel because uncomfortable sobriety is the logical conclusion of not getting your needs met for those nutrients.”
“How you feel is data” – illuminating chart by The Suppers Programs. Click on image to view a high resolution PDF.
If you think you are experiencing a link between hypoglycemia and alcohol, seriously consider cutting down or, under professional guidance, stop alcohol consumption altogether. Then start focusing on your dietary and nutritional deficiencies that you may have as the result of your drinking (or the cause of it), and work toward consuming a balanced, nutrient-rich diet that will restore your health and stabilize your blood sugar. Consider the following basics:
- Eliminating simple carbohydrates from your diet, especially highly-refined and processed carbohydrates that are quickly absorbed by the body.
- Replacing simple carbohydrates with more complex carbohydrates, that can be found in foods such as whole grains and vegetables.
- Adding healthy proteins and fats to your diet since carbohydrates are absorbed more slowly with fats.
- Not skipping meals. Instead eat at regular intervals throughout the day to regulate blood sugar levels.
Please see your health care practitioner for further evaluation and a treatment plan.
We hope this brief introduction to the relationship between hypoglycemia and alcoholism has been helpful.
Here are a few resources, links, and suggestions to help:
- Visit hypoglycemia.org and check out our Diet Suggestions, one of the best tools to control hypoglycemia/alcohol symptoms. A hypoglycemia diet and lifestyle change may be just what you need to keep you on the road to recovery.
- Consider joining our private Hypoglycemia Support Group – you aren’t alone in this struggle, why not join with many others who have walked in your shoes.
- Educate yourself thoroughly on the correlation between hypoglycemia and alcoholism by reading Julia Ross’s books, Mood Cure and Craving Cure, Seven Weeks to Sobriety: The Proven Program to Fight Alcoholism by Dr. Joan Mathews Larson and Under The Influence by Dr. James Mylam.
- Look into the work of Dr. Barbara Reed Stitt, author of Food and Behavior. Stitt, a former Chief Probation Officer, writes and speaks about her years of research and experience with correcting behavior by modifying diet.
- If you live in or near New Jersey, you can get involved with Suppers Programs meetings. Suppers is a network of nearly free-to-users programs where people cook together, eat together and support each other’s personal pathways to a healthier life.
- Set an example if you are a parent. We cannot tell our children to “just say no to drugs” (alcohol, sugar, etc.) if we ourselves are not role models.
- Make sure your children are supervised. The greatest risk occurs when children are left alone.
- Get your child involved with after-school activities.
- Recognize the warning signs of alcohol and drug abuse in children: decline in grades and school attendance; discipline problems; changes in attitude, friends, and physical appearance; and most importantly, physical conditions such as loss of appetite, excessive fatigue, and sleeping habits.
- Recognize the warning signs of alcohol abuse in adults: personality changes, high absenteeism on the job, low productivity, confrontations at work and home, and increased sleeping habits.
- Recognize that most, if not all, alcoholics are hypoglycemic, and unless both issues are addressed, recovery is severely hampered.
If you or someone you know has a problem with alcoholism, please don’t stop here.
The information presented here is to plant a seed, give you hope, encouragement and knowledge that this disease needs to be looked at from every angle if success is to be achieved. Take this information and delve further…for the life you save may be your own.