The Freestyle Libre Can Liberate You
Self-Monitoring Technology Can Help Maintain Metabolic Health and Control the Blood Sugar Roller Coaster
The Hypoglycemia Support Foundation is blessed with an amazing group of medical advisors, including Dr. Mark Cucuzzella. One really hot topic right now is the use of Continuous Glucose Monitors (CGM), which have traditionally been used by Type I Diabetics for years. While most insurance companies do not currently cover the expense of the devices, the costs have come down and the technology is more available than ever for non-diabetics. Many doctors have been adopting the technology for themselves and their patients. Here is a fantastic in-depth article by Dr. Cucuzzella describing his experience with one of the devices: the Abbott Freestyle Libre.
The Freestyle Libre Can Liberate You
By Dr. Mark Cucuzzella
One of the most empowering and liberating self monitoring devices I have ever used for myself and for patients is the continuous glucose monitor or CGM. Just as the simple glucometer now is readily accessible and affordable to all without a prescription, the time is coming soon where this will also be true of the CGM. A CGM measures glucose continuously with immediate results beamed to your phone or small reader. A colleague of mine, Dr. Dan Cox, University of Virginia, is a psychiatrist researching CGMs and he empowers patients by placing the tool in the patient’s hand to make change. [Two good articles from Dan are here and here]. The experience can be liberating since the CGM can show you exactly what happens with foods that many believe to be safe but yet still have natural sugar and drive hyperdopaminergic responses (dopamine-driven disruptive deficits in decision making) that hijack your brain. With the CGM barking at you in a friendly way, you can finally liberate yourself from these foods and addictive metabolic states of being.
My introduction to a CGM occurred in 2012 when at age 45 I was identified with an elevated glucose and Hemoglobin A1c (3 month average glucose) on a military physical. I did not fit the profile of the usual middle-aged male or female who presents with high sugar along with other common metabolic suspects of central obesity and high blood pressure. The patients fitting this profile often have high insulin levels and Insulin Resistance and are on their way to Type 2 Diabetes. Another colleague of mine, Dr. Jason Fung, describes the issue of insulin not being able to move any more glucose into the cells with the metaphor that “they cannot stuff any more shirts in the suitcase” – causing the glucose to creep up in the blood. To understand Insulin Resistance and its relevance to almost all modern chronic disease you must dig into the work of pioneer researcher Dr. Gerald Reaven who recently passed at age 89 with nearly 1000 scientific papers, chapters, and books to his name.
Even though I presented with similar high glucose readings as folks in this category, I was lean and still running marathons and ultra races in my mid 40s. After a battery of tests I came back with a low c-peptide insulin level. This is a scenario where you are becoming insulin deficient as opposed to hyperinsulinemic (high insulin levels and Insulin Resistance). There are several non-specific names for this condition – none of which identify the root cause. It can be referred to as Latent Autoimmunity Diabetes of Adulthood (LADA), Maturity Onset Diabetes of Youth (MODY), or the even more non-descript Type 1.5 Diabetes. In most cases when a person continues exposure to the same environment and foods it will progress to a Type 1 equivalent and a reliance on insulin therapy.
As chance or luck would have it, this was occurring at the same time I was doing a deep dive into obesity in the military as it related to passing or failing the fitness test. This article by Gary Taubes changed my life and led me to read dozens more books and 1000s of scientific papers on root causes of obesity and diabetes. Probably even more fortunate was access to test an early model Dexcom CGM at the base where I was stationed. The base was using this for some research and, as a doctor, I knew of it and asked to try it. The device has a small catheter that inserts under the skin on the belly and the readings went to a pager like device. I wore the device for 3 days before turning it back in.
What was shocking at the time (not so much now after learning about glucose response to carbohydrates) was the super high and immediate glucose rise well over 200mg/dl with any cereal or bread product in small serving size quantities. These rises were usually followed by sharp declines and a feeling of uneasiness mentally and physically and a bit of what is commonly called “hangry” (hungry+angry). I had been a monster cereal eater for breakfast, meals, evening snacks, and even middle-of-the-night snacks for years and had not been feeling well for the previous year. When cereal was not the entrée it was bread or pasta. I had sworn off eggs and most meats since the government and heart specialists gave them the lethal tag and with my father needing a bypass at age 35 and a redo at 45 I heeded this flawed advice.
During the short 3 day experiment I did try some eggs and there was no rise in blood sugar and I even dipped into former forbidden foods such as bacon with similar encouraging results. Some fruits gave significant rise but I did not have time to fully test many varieties in the 3 days. The CGM trial did convince me that food really mattered and I purchased a glucometer to continue the testing old school fashion with frequent finger sticks and I have tested thousands of times in the last 7 years in order to sort it out.
People say coming off grains is hard but when one sees the effect it has on blood sugar, especially if you have any type of diabetes, the decision is an obvious one out of necessity. Thus, since 2012, I have followed podcast friend Vinnie Tortorich’s NSNG rule (No Sugar No Grain) and my A1C has come down from above 6 to near 5 with no medication. I think the CGM saved the life of my pancreas and liberated me from grains. Yes, liberated me. There is no moderation if a substance is causing harm and feeding more addiction. For me as well as for much of the population, sugars of all forms light up the addictive parts of the brain like the Fourth of July.
Fast forward to 2019 and the world of accessible and affordable CGMs is upon us. Through a small sensor catheter CGMs read glucose from the interstitial fluid which is a close reflection of capillary blood glucose (fingerstick). There are two high end and expensive versions mostly geared to people with Type 1 Diabetes – Medtronic Gaurdian and Dexcom G6 (the most current model). These are precise enough within a 3% margin of fingerstick glucose. The Medtronic requires twice a day cross calibration with a glucometer but the new Dexcom G6 does not require this.
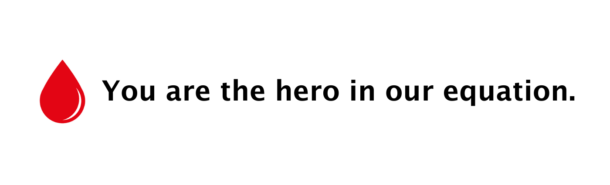
The true disruptor in the CGM space is the Abbott Freestyle Libre. This entry level device is available for about $60 per 2 week sensor (try goodrx) and with free apps or iphone (7 or higher) or android it can make direct communication with your, negating the need for the $70 reader and another device to carry. Abbott offers “LibreView” and also Tidepool offer online tools for uploading, tracking and interpreting data and producing insightful reports. A plus is the extreme ease of insertion and use as well as the affordable cost. A con is the accuracy can be off by 10%, but unless you are precisely dosing insulin this small variance doesn’t negate any practical reason to not learn from and follow the glucose trends. It also does not have alarm functions. Many patients are diagnosed with Type 2 Diabetes with a single blood sugar (see ADA criteria). Many take meds and think they are managing their diabetes and never check blood sugar. One isolated blood sugar reading would be similar to one blood pressure reading, which most would agree is not enough information to make long term diagnosis and management decisions.
So What Does Freestyle Libre Look Like and Where Does It Go?


Photo credit to my son Leo who took these pictures while on vacation in Glacier National Park.
The Freestyle Libre, like other CGMs, is a small button with a tiny catheter that you insert usually on the back side of your arm. Some prefer the abdomen. It takes about a minute to insert it and it stays on for 14 days. I cover mine with a waterproof patch called Simpatch which allows you to swim, get sweaty, and avoid knocking it off during activity. I lost my first one doing Burpees with a tegaderm tape which was not robust enough. A product called “skin prep” or “benzoin” can help make your skin a little tackier for durable adhesion.
For those who do not like reading directions here is a video I made on how to install the device:
So here is a bit of good, bad, and ugly of my recent Freestyle Libre experiment.
Note: this is my physiology and might be completely different that yours. I’m using these examples to share how the CGM can give you very useful information specific to you. And you are what matters when it comes to any medical advice or treatment.
The Ugly
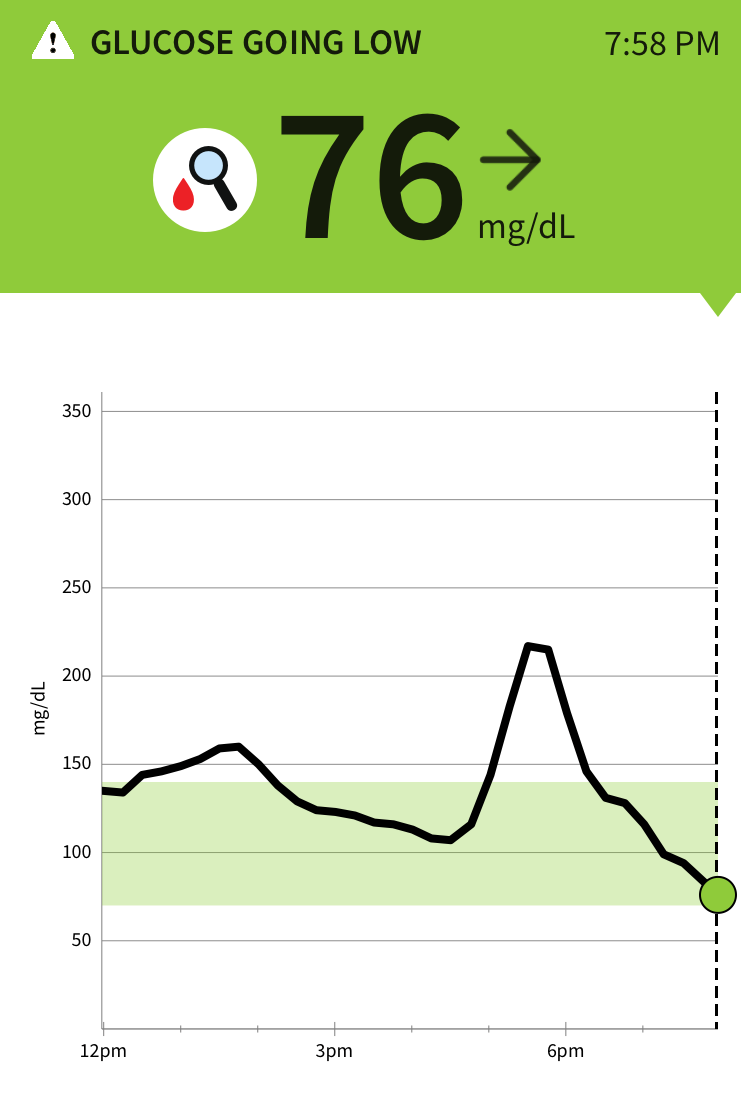
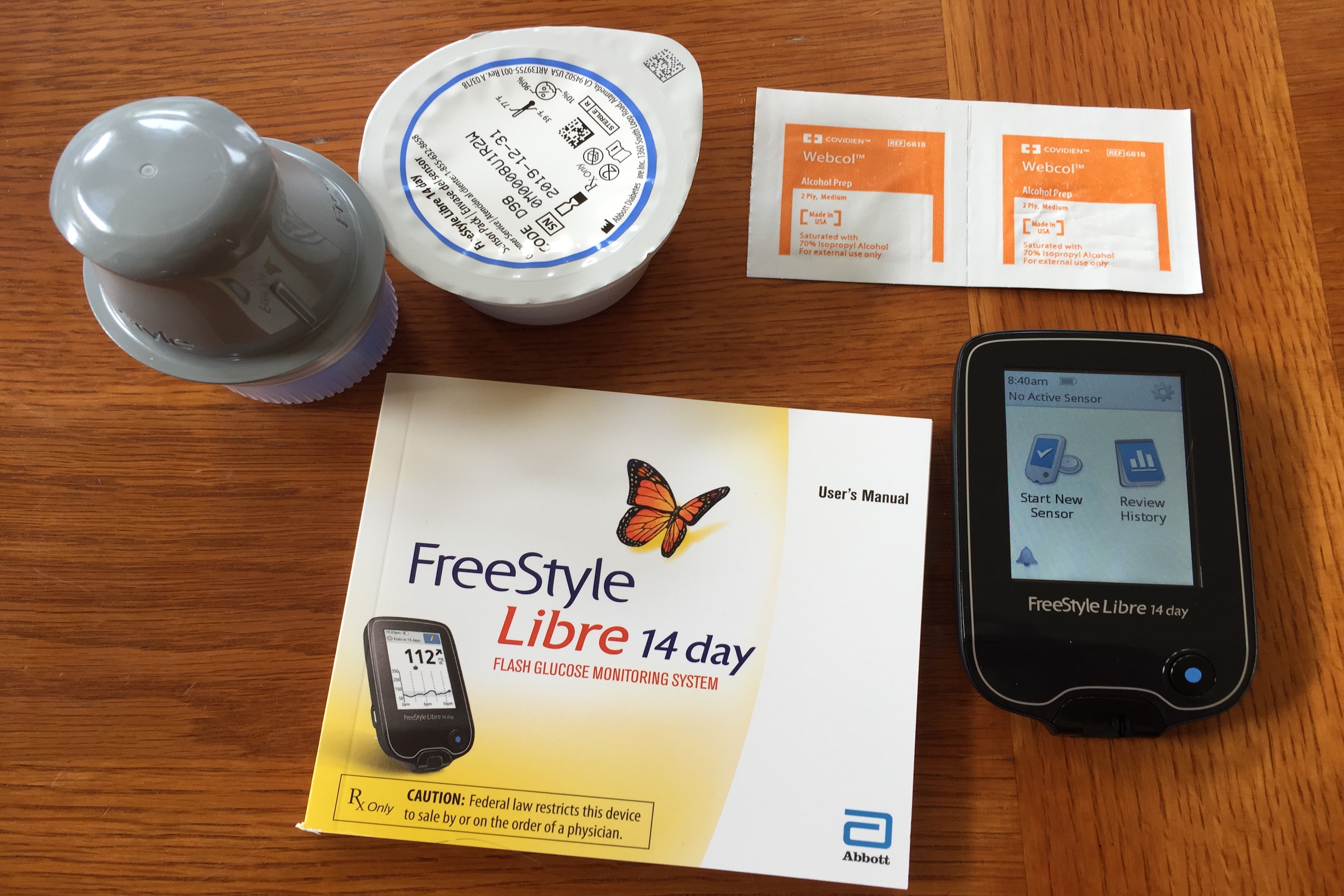
These images show my glucose response to 4 small (large marble size) “sugar free” date and nut balls. I was curious how the fat from the nuts as well as higher fructose vs glucose would affect this. Fructose (fruit sugar) has a first pass through the liver and slower hit to the bloodstream versus glucose (refined grains/flour products) which are immediately absorbed. Fat usually slows glucose absorption. I estimated the carb content of the 4 balls was about 30-40g total. The little bump into the 160s at 1pm was half a Kind bar snack. What feels horrible is not so much the high but the crash afterwards. To explain this phenomena, I lack a sufficient first phase insulin response but am highly insulin sensitive. I likely make a second phase insulin response which kicks in a couple hours after the carb ingestion and can overcorrect. How does one feel when their sugars drop so quickly? To me it is a migraine type headache, nausea, irritability, inability to concentrate, and a bit clammy and sweaty. To put the carb count into perspective many patients with Diabetes Type 1 and 2 are advised to have 60 grams of carbs per meal (equivalent of 2 pieces of bread) and 15 grams per snack. Pregnant women drink a 50g glucose drink and if their value is above 135 they are in the Gestational Diabetes range and need further assessment. Imagine how the curve would look with the often suggested 60g carb load? I’m not doing that experiment again I saw the result in 2012 and on this day saw the effects of half this amount….ugly.
Fortunately, the 2019 ADA position paper on Medical Nutrition Therapy allows a low carb option which I believe should be offered to all patients as an option with the tools for them to self-assess, empower, and liberate themselves to make informed decisions on their own care.
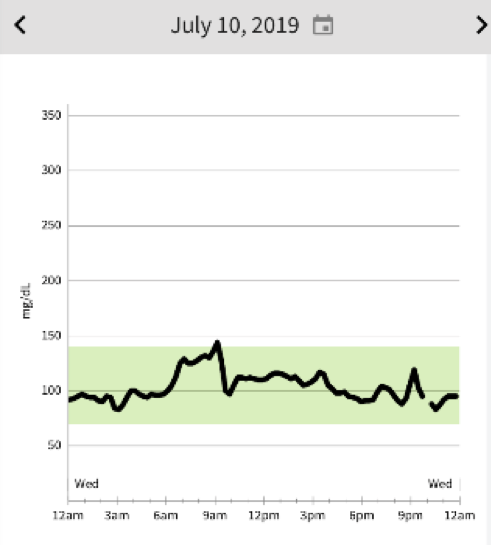
The Bad… Although the Mango was worth the rise and fall!
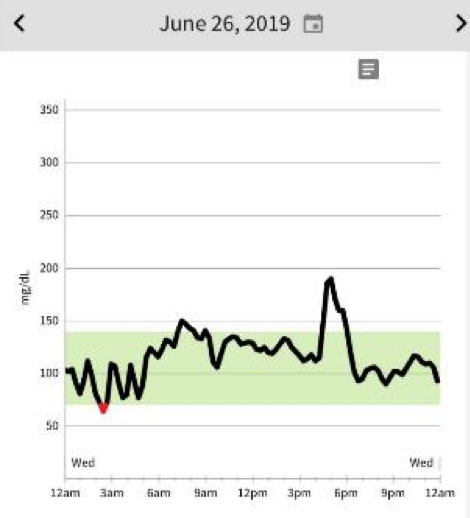
This is a 24 hour graph from the Libre app. My wonderful friend David Greenfield from Miami grows the most amazing mangos in his yard. David came up to our adult run camp in Shepherdstown. Maybe a better description would be adult run/play/enjoy local food and drink camp. This glucose spike was from the most delicious mango I have ever tasted. The single mango did not result in the same rise and drop as the dates but imagine if I ate 2 of them. Trust me, these mangos can be addictive (they are that yummy) and if your metabolism can handle it then they are a healthy choice but if it cannot the fruit needs to be viewed as “nature’s candy”. Depending on how you view things you could say “like candy I will enjoy an occasional treat” or “I have diabetes and do not eat candy”. If David returns with these again I will have just one. A couple other things to note on this graph is the night low and morning rise with exercise (I exercised from 6am to 730am) which we will get into on a later graph.
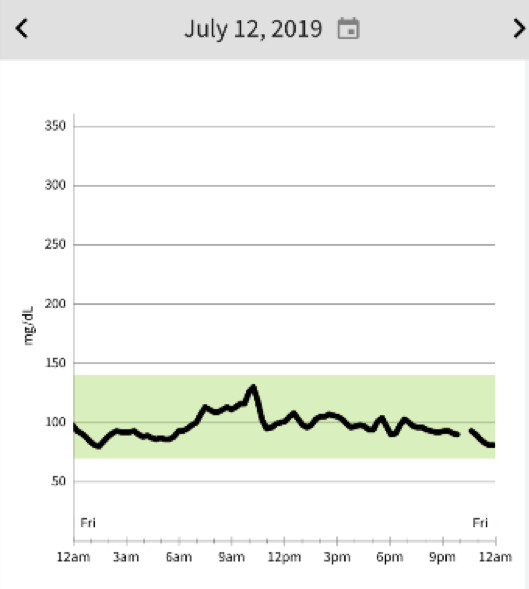
The Bad- Reactive Hypoglycemia
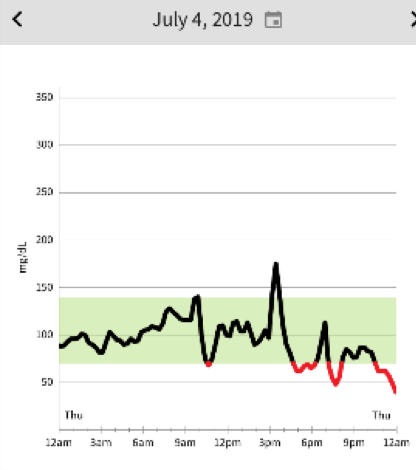
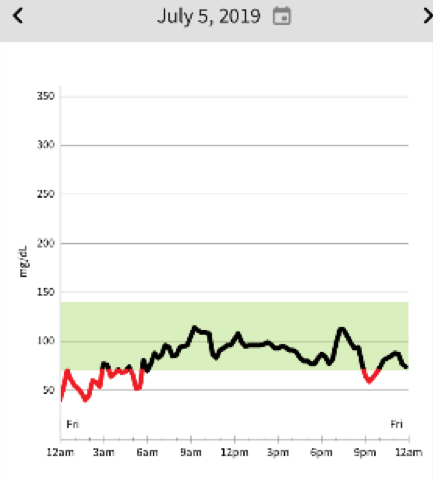
Here are tracings from the 4th and 5th of July. After a some wonderful holiday stand up paddle boarding on the Potomac River with my kids, we enjoyed a small watermelon snack about 3pm. My serving was about a one-inch quarter wedge. Feeling a bit hangry I enjoyed a bit more fruit salad at a 4th of July picnic 6 o’clockish. I slept very restlessly that night, waking a few times kind of clammy and went back to bed. The next morning I scanned the Libre and it showed several drops to the 40 range. Conventional advice would be take in some sugar and not exercise. But since taking in sugar can cause me to have more reactive hypoglycemia, and exercise raises my blood sugar, I decided to go for a fasted run from 7 to 8:30 am with the resulting rise in blood sugar and restored good feeling.
Note of caution: If you are using insulin therapy or a sulfonylurea medicine you do need to take in a measured amount of glucose as the medicine is driving the sugar down. I am not on medication, and I am not advising anyone to ignore directions from your doctor or healthcare provider. This is my personal story, not a one-size-fits-all guide for everyone reading this article.
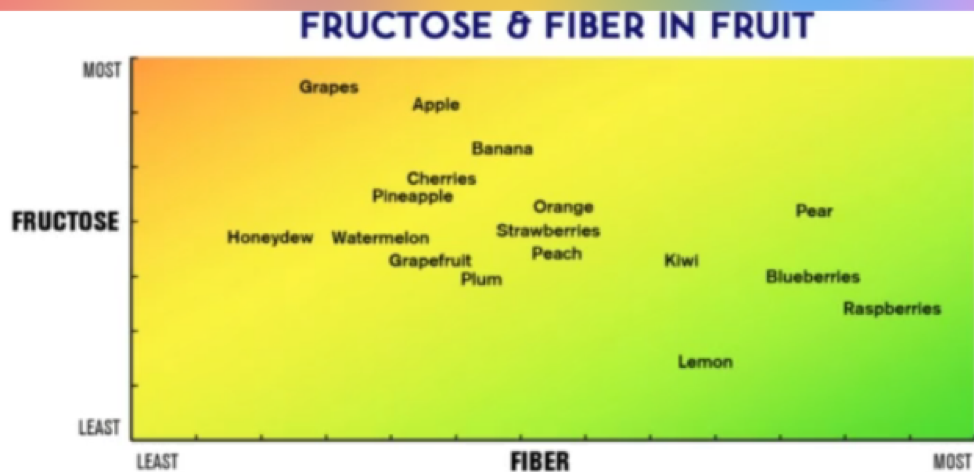
This is a useful chart on fruit but your results are unique to you. A general rule is more fiber and less fructose will have less impact on your blood glucose, but individual results may vary.
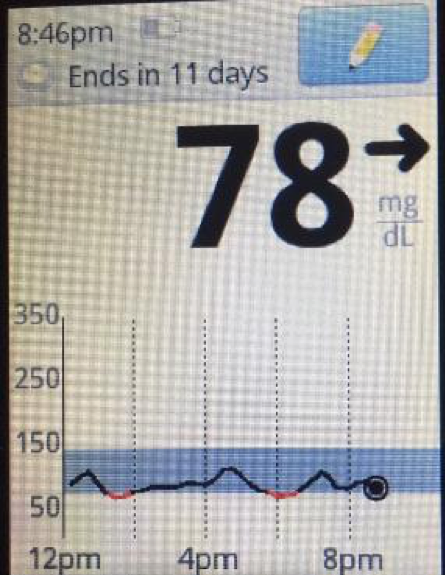
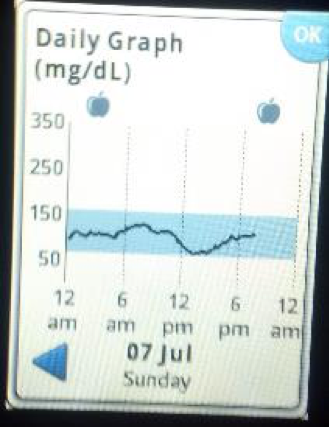
This image from a friend’s Libre reader shows low oscillation reactive hypos. She eats an amazingly healthy diet. If she were having any physical or mental symptoms during the times in the red she would need to go back and assess the meal. We advise patients to check sugars before meals but as you can see the isolated tests would completely miss the lows.
An amazing resource for hypoglycemia is The Hypoglycemia Support Foundation. I am a medical advisor to this foundation along with some amazing mentors, clinicians, and researchers in this area. See the infographic and get a better understanding of hypoglycemia and causes – their metaphor of the “blood sugar roller coaster” brings light to the relationship between high and low blood sugar. They also offer a diet symptom diary, an extremely useful tool for correlating data from CGMs with what you eat and symptoms you experience.
Now The Good – When You Become Empowered and Liberated It’s All Good
A Good Night’s Sleep with Stable Blood Glucose Starts with a Stable Day Before
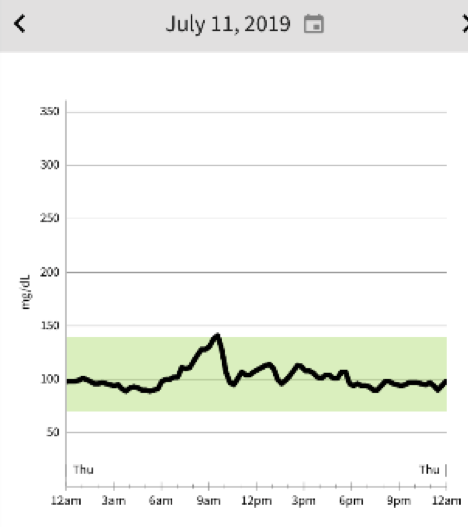
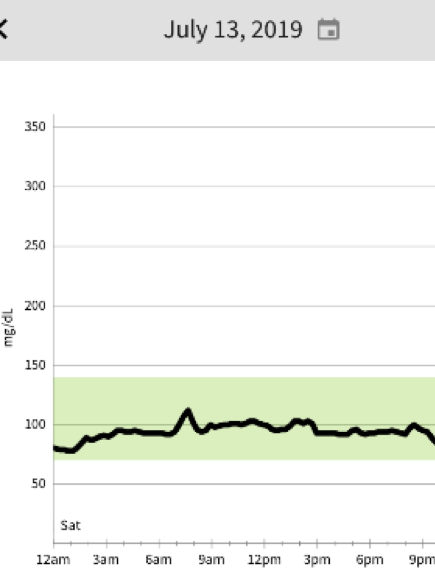
See this sequence of days when food behaving on vacation in Glacier Park and probably taking in no more than 30g of carbs a day with average daily running and walking mileage 17-20 miles at altitude. As I’ve done for the last 6 years, I start each day with the usual 4 egg omelette with veggies, cheese, meat, and veggies. This is medicinal for as it creates satiety, stable blood glucose, stable physical energy, and mental clarity. Lunch is usually something simple like chunk of cheese and maybe some nuts, and a standard dinner would be a monster salad with a good quality protein (meat or fish) and lots of Extra Virgin Olive Oil. Dry red wine has no impact on my blood glucose and I really enjoy it. Red wine would be hard to give up. Beer is like bread. What you notice is what you typically don’t notice without a CGM…..where are the meals on the curves? The only predictable rise is with the morning run. July 13 there was no morning run as this was long hike day. Even with physical activity, there is usually a small rise in the morning with the cortisol response.
Stable Sugars Hiking 16 Miles

Here is the glucose graph from what my kids described as an epic hike in Glacier National Park in July. 16 miles and 8 hours on the Highline Trail and spurs to high passes (picture of my children Leo age 16 and Lily age 14 on Swiftcurrent Pass). It is liberating to be able to do this knowing you will have stable sugar and energy. Here are a few tips.



My kids packed the usual pizza, some cookies, and chocolate. They do not have my sugar issues so it’s all good and they would be burning lots of sugar on the trail. I burn fat so I packed some happy fat- bacon, cheese, and roasted nuts. Another key to feeling good on long duration activity is adequate salt. Insulin is a salt retainer and when you are low carb and low insulin you need the salt. At home I use a product called UCAN Hydrate. I forgot my packets so I made do with a mixture of Pink Himalyan Sea Salt and pinch of organic lime juice. I make a concentrate and put it in a single bottle and then add this to bottles of free water so all water has some salt and very diluted juice for a little yummy flavor.


I own a small shoe store called Two Rivers Treads selling only natural footwear (flat and wide) so here are the obligatory product placement shots. Shoes are Merrell Vapor Gloves (Lily), Altra Superior (Me), New Balance Minimus (Leo), Injinji Toe Socks, Correct Toes (if you have Hallus Valgus as I do), and the colorful Cotapaxi pack.
Travel Days Are Good Days If You Prepare And Know Your Numbers
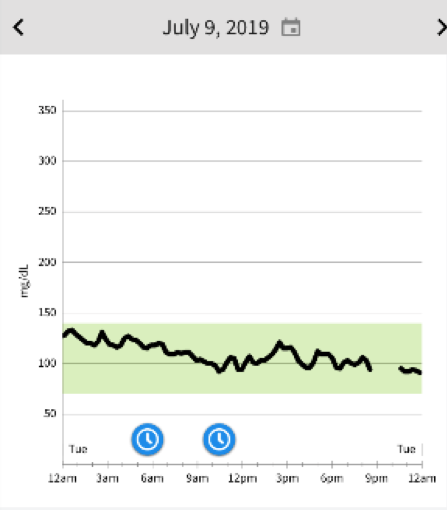

Here is a picture of TSA friendly low carb foods to get you through a 12 hour travel day getting to your destination. I only had the cheese and saved the nuts and chocolate for later. The Libre shows it is possible to not go off the rails when traveling and succumb to the airport food and pretzels and biscuits they serve on the plane. The blue clocks are time zone changes. The LibreView app is pretty smart.
Making Sugar When You Exercise Is A Good Thing
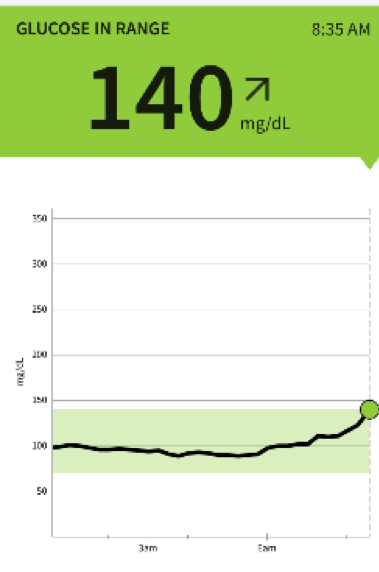
The graphs above show what typically happens on a morning run (glucose rises) followed by a 4-egg omelet (glucose falls). In the summer, I especially like to run in the early morning. It’s cool. I always run fasted not counting the non-negotiable black coffee. When insulin is low the body has two primary processes to make glucose. There is only 4 grams of sugar in the bloodstream controlled by a masterful dance between Insulin and its counter regulatory hormone Glucagon.
When Insulin is low, Glucagon can become active and allow these processes to occur which is a good thing if you want consistent sustainable energy. You do not need to eat glucose to maintain blood glucose, your body will make it if you train it to.
Why does the glucose fall after a large breakfast loaded with healthy fats and protein with a little non-starchy carbs from veggies? I believe this has to do with the insulin sensitivity from exercise and when the exercise ceases, the gluconeogenesis and glycogenolyisis ceases, and the muscles and liver then soak up the glucose from the bloodstream. This occurs at the same time as I’m eating omelet which has about 800 calories with maybe 5% are non starchy veggie carbs.
Note: By the ADA criteria of fasting glucose (greater than 126) I would be diagnosed with full blown diabetes with the fasting glucose of 140, as mine often is after a fasted morning run. My last A1C in 5.2 so I and many others I see, know that I have Diabetes in remission.
For the deep science dive into this read the 2008 paper “4 grams of Glucose” from Vanderbilt team.

Here is the delicious medicinal omelet which gives satiety and energy for a full day. See how many fresh ingredients you can identify?
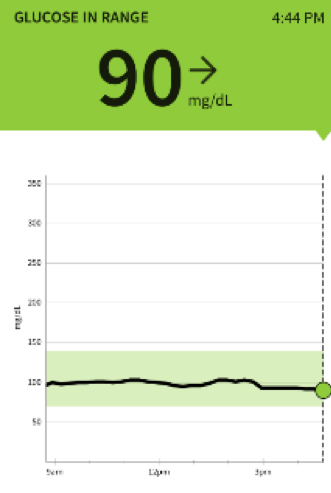
Achieving a No-Hitter
Some of my patients are now using the FreestyleLibre. Friend and colleague Dr. Jake Kushner who specializes in pediatric Type 1 Diabetes describes a day when your sugars are 100% in the safe range as a “no hitter”. Here are a few images of a patient who 6 months ago was averaging sugars in the 300s. He has dramatically reduced his diabetes meds, lost weight, regained energy, and is making a fun challenge to pitch “no-hitters”.
Screen shot and quote from patient VH
“One hit day after breakfast (v8 juice?- no other carbs unless a plain latte?). Experiment continues. The libre encourages me that I’m making progress. Didn’t need any humulin [short acting insulin]at all today.”
Lesson learned– yes V8 is sugar.
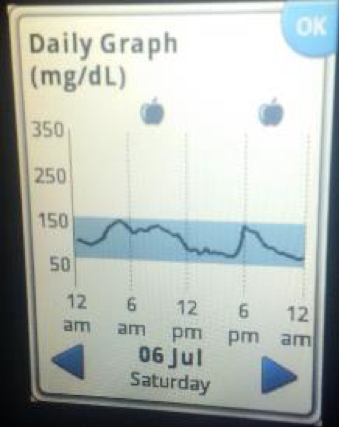
VH gaining control
“Had a no hitter yesterday despite attending a pool party with tons of carbs (which I politely declined :)“
VH staying on the plan
“Another no hitter.”
Text to me July 15 “Things going well. 5 or 6 days no-hitters”
Practical Tips for the Libre
Ask your doctor for one if you have pre-diabetes or diabetes. If your insurance does not cover it is worth the $60 bucks for two week trial to learn something about yourself.
Although not as accurate as the Medtronic or Dexcom, The Libre is the simplest and best entry into the CGM world.
- The Freestyle Libre is not a real time CGM with alarms like the Dexcom and Medtronic so view it more like a replacement for multiple finger sticks.
- The Freestyle Libre reading is an average of your last 10 minutes so it is not complete.
- One way to do the experiment is eat a week or at least a few days with your usual pattern. Note the effects of different foods, exercise, sleep, even stress. Then make a meaningful change and be consistent for a week. Change one variable only and I suggest change the food. Keep your regular activity patterns. How do you feel? Are you hungry? How are your blood glucose readings?
- Download the free Freestyle Libre Link app to your cell phone then you do not need the reader. Some thick cases will block the signal. The iphone reads from the top of the phone. I have a pretty beefy Otterbox and it still works.
- Clean and dry skin with alcohol wipe to remove any oils and apply a waterproof adhesive patch like Simpatch. There are even fun colors from a site Pimp My Diabetes. There are also small armbands your can wear to secure the Freestyle Libre or other CGM devices.
- Cross check with your glucometer. This is a must. From the experience of folks using these frequently the reading may be a bit off in the first 12 hours and then again on the waning day or two of the sensor. I have seen some variance up to 15 mg/dl cross checking with my glucometer and these are usually on the extreme high and low ends of readings. If a reading does not seem to make sense cross check with glucometer. Cross check every new sensor. Sensors can have their own personality and even a variance on the placement position can matter. Alternate arms every 2 weeks. Or try some different sites (here is a relevant and fun video).
- CGM measures interstitial fluid not capillary blood and there is about a 10 minute lag to see the CGM change. So the times this has relevance is when you are rapidly rising and rapidly falling.
- Figure out what 1 g of carbs does to your blood sugar. For me and many with Type 1 diabetes, 1 g of carbs raises me 4 so 30g will raise about 120 as demonstrated by the date ball experiment.
- Make a daily goal of a “no hitter” (staying in the safe range 70-140) and if you fall out of that range figure out why
- Find a healthcare provider who will partner with you to help
- Have fun with this as you experiment and share your results and share readings with others doing the same. Everything I have learned has been from patients and from self-experimentation. And the experiment never ends
Final Thoughts
In an old business classic “The Innovator’s Dilemma “ there is discussion of disruptive technology versus sustaining technology. I place the CGM in the sustaining technology category. Scholar and innovation expert Clayton Christensen explains it this way.
“A sustaining innovation targets demanding, high-end customers with better performance than what was previously available.”
The CGM is a vast improvement over old school methods of monitoring diabetes and giving the patient the information they need to make daily adjustments in their continuous journey to better health. There is no finish line.
If you need help in this area I see patients at
WVU Center for Diabetes and Metabolic Health
304-596-5038
Endnotes
For a little more on the clinic approach to diabetes metabolic disease I would like to share this one hour interview I did a couple months ago for a project called the Kick Sugar Summit which involved healthcare providers as well as advocates and policy makers from around the world. Even locally there is a lot of confusion and even misinformation about what I try to do. People have mentioned even to me directly that I tell people never to eat carbohydrates and only to eat from certain food lists. This is absolutely not true I think this interview explains the process of how we can engage and empower patients to make change. The approach is designed in the model of self-care in addition to healthcare, achieving self-efficacy, approaching the problem with compassion, individualization with a scientific approach, simple self-quantification (i.e. glucometer), the brain and addiction, and there is no finish line. I discuss some of the controversies and current literature. At the end, I bring in the power of teamwork and mention the work of my colleagues at the WVU Center for Diabetes and Metabolic Health as critical partners all doing unique and essential work. This dropbox link allows you to download an audio file which you could even put in iTunes and load on phone to go for a walk. I have done lots of podcasts and webinars and this one actually turned out pretty well from a provider perspective without any specific agenda from the interviewer.
- www.tinyurl.com/MarkKickSugarSummit – This webinar recording is about hospital, local community, and system based change relevant to our state. It was hosted by Canada’s IPTN
- https://www.therapeuticnutrition.org/ – Run by physicians and pharmacists north of the border.
- https://youtu.be/CUvateyxsGc – This blog describes the process of low-carbohydrate and athletic performance
- http://naturalrunningcenter.com/2017/03/07/burn-fat-health-performance-better-butter-burner – What is the ideal way of eating to sustain human health as well as protect the environment? There is also a lot of controversy about the environment and sustainability of food systems and this blog shares many links to allow people to make informed decisions on the topic. Need to get rid of the processed junk!
- http://naturalrunningcenter.com/2019/01/27/eatlancet – The WHO withdrew support
- https://www.bmj.com/content/365/bmj.l1700 – The 2020 Dietary Guidelines are soon to be released.
- I summarized my thoughts on the importance of getting this right after the release of the 2015 Guidelines – http://naturalrunningcenter.com/2016/01/17/2015-dietary-guidelines-america-sailing-safe-harbors-keeping-full-catastrophe/
- For a detailed review of Insulin Resistance for the scientifically minded written by friend and colleague Dr. Tim Noakes with tribute to Dr. Reavan, check out: https://www.crossfit.com/
essentials/its-the-insulin- resistance-stupid-part-1 and here https://www.crossfit.com/ essentials/its-the-insulin- resistance-stupid-part-2 - A few downloadable published articles I have written with colleagues on the topic
Many thanks to the readers for your passion in this area.